Pelvic floor reconstructive surgery consists of several procedures for correcting a condition called “pelvic organ prolapse.”
When the muscles of the pelvic floor are damaged or become weak – often due to childbirth – they are sometimes unable to support the weight of some or all of the pelvic and abdominal organs. If this occurs, one or more of the organs may drop (prolapse) below their normal positions, causing symptoms including discomfort, pain, pressure and urinary incontinence.
The goal of pelvic floor reconstruction is to restore the normal structure and function of the female pelvic organs.
About 35 percent of women will develop some form of pelvic organ prolapse. The condition can often be treated with nonsurgical therapies, but it sometimes requires pelvic floor reconstructive surgery. The expertise and skill of the physician is extremely important in these procedures.
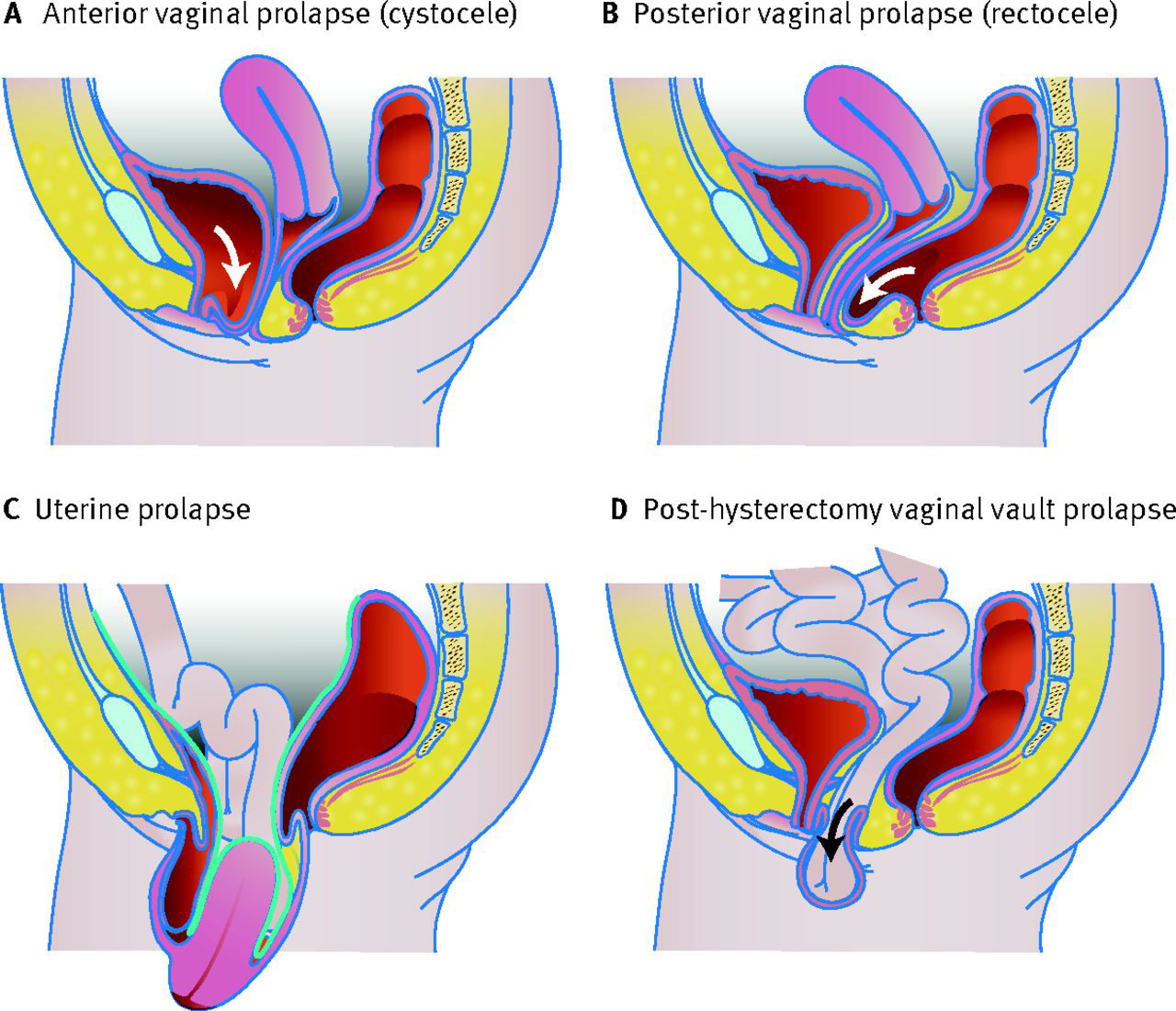
The pelvic floor consists of the muscles, ligaments, connective tissue and nerves that support and control the rectum, uterus, vagina, and bladder. This “floor” can be damaged by childbirth, repeated heavy lifting, chronic disease or surgery.
Pelvic floor dysfunction can lead to:
Incontinence – Loss of bladder or bowel control and leakage of urine or feces.
Prolapse – Descent of pelvic organs including dropped uterus, bladder, vagina or rectum. About 35 percent of women will develop some form of pelvic organ prolapse.
Emptying disorders – Difficulty urinating or moving bowels.
Pelvic pain – Discomfort, burning or other uncomfortable pelvic symptoms, including bladder or urethral pain.
Overactive bladder – Frequent need to urinate, uncomfortable bladder pressure, urge incontinence and difficulty holding a full bladder.