What Is Intrauterine Insemination (IUI)?
Intrauterine Insemination (IUI) Russian/Ukrainian Speaking Clinic for New Jersey patients
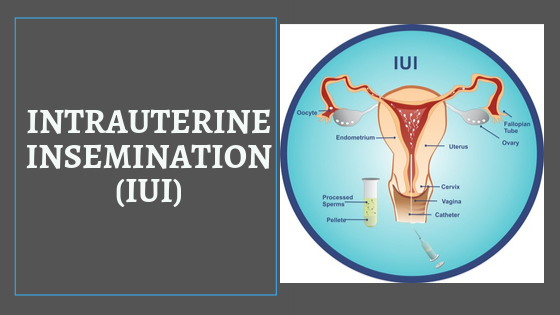
IUI, or intrauterine insemination, is a relatively simple fertility treatment. It may be done with or without fertility drugs. The procedure itself involves transferring semen that has been washed and concentrated directly into the uterus via a thin catheter. IUI is done around the time of ovulation or in conjunction with fertility drugs to maximize the likelihood of conception.
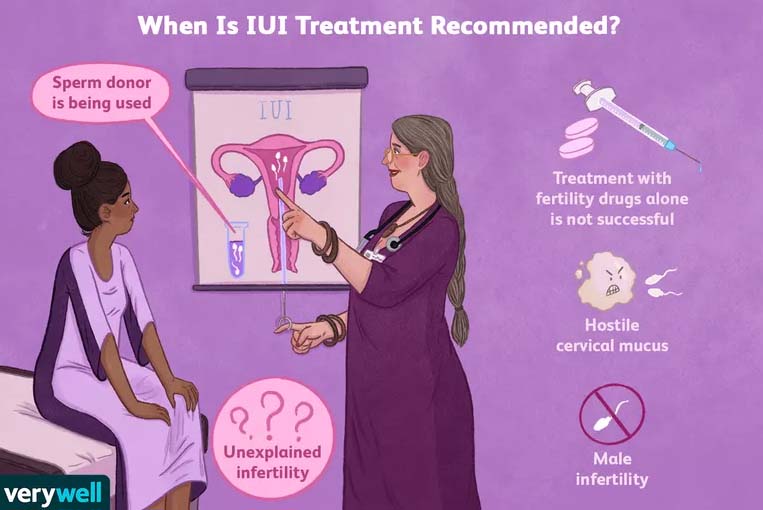
When It’s Used
IUI is used to treat many types of infertility and is often done in multiple cycles until pregnancy is achieved—or another treatment is tried. IUI is often the first procedure tried before moving on to more invasive options, such as in-vitro fertilization (IVF). Some insurance companies require a few cycles of IUI before paying for IVF.
Cycles of IUI may be recommended to treat any of the following infertility situations:
- Hostile cervical mucus
- If a sperm donor is being used
- If sexual pain makes intercourse not possible
- If treatment with fertility drugs alone is not successful
- Male infertility
- Unexplained infertility
IUI is not recommended for those with:
- Blocked fallopian tubes
- Previous pelvic infection
- Severe endometriosis
Treatment Cycles
Your treatment cycle (and how many cycles you plan to do) will depend on why your doctor has recommended IUI and on whether you’re taking fertility drugs. Two common treatment cycles that do involve fertility drugs include:
Clomid or Letrozole with IUI
IUI may be added to a Clomid or Femara (letrozole) treatment cycle. In this situation, as soon as your next period starts, you’ll have a blood test. You may also have an ultrasound. This is to confirm you’re not pregnant and don’t have any ovarian cysts.
Assuming everything looks good, you’ll start taking the oral fertility drugs on the days prescribed by your doctor.
Gonadotropins with IUI
Gonadotropins are injectable fertility drugs, including FSH, LH, hMG, and hCG. Brand names you may recognize are Gonal-F, Follistim, and Ovidrel. When you get your period, you’ll call your doctor to schedule a baseline ultrasound and blood work. (As mentioned above, these tests are to confirm you’re not pregnant and don’t have any problematic ovarian cysts.)
You’ll start giving yourself fertility drug injections according to your doctor’s instructions, and you’ll have transvaginal ultrasounds and blood work throughout treatment.
The transvaginal ultrasounds will look for developing ovarian follicles. The ultrasound tech will look to see how many are there, how quickly they are growing, and whether they are nearing maturity. The blood work will measure estradiol (E2), LH, and progesterone.
Your medications may be adjusted based on your hormone levels and the size and number of follicles growing on your ovaries. When one or more follicles reach maturity, your doctor will schedule a trigger shot of hCG to prompt the ovaries to mature and release an egg. Then, you will schedule the IUI procedure.
IUI Procedure
For the procedure itself, you will lie down on a gynecological table, similar to the ones used for your yearly exam. A catheter—a small, thin tube—will be placed in your cervix. You may have some mild cramping, similar to what you might feel during a Pap test. The specially washed semen will then be transferred into your uterus via the catheter. Then, the catheter is removed, and you’re done.
Your doctor may suggest you remain lying horizontally for a short while after the procedure, or you may be able to get up right away. In either case, you don’t need to worry about the sperm falling out when you stand up. The sperm are transferred directly into your uterus. They aren’t going anywhere but up to a (hopefully) waiting egg in your fallopian tubes.
How Soon After Sex Do You Actually Get Pregnant?
After the Procedure
After the IUI procedure, you may be prescribed progesterone. This is usually taken via a vaginal suppository. About a week after the IUI, your doctor may order blood work. They will check your progesterone levels, estrogen, and (maybe) hCG levels.
Your doctor may order a pregnancy blood test ten to 14 days post-IUI, or they might have you take an at-home test. Waiting to find out if the treatment was successful can be very stressful. Take good care of yourself.
Risks
IUI is a relatively low-risk procedure. There is a very small risk of infection.1 Some of the biggest risks come from the fertility drugs used. If you’re using gonadotropins, you may be at risk for having a multiple pregnancy or developing ovarian hyperstimulation syndrome (OHSS).
Multiples
Your risk of conceiving multiples (twins, triplets, or even more) is higher when taking gonadotropins. This is why monitoring is important. If there are too many potential follicles, the cycle may be canceled and tried again at another time.
Ovarian Hyperstimulation Syndrome
If your doctor cancels your cycle because there are too many follicles (more than 20), they will also likely tell you to abstain from sexual intercourse. It is important to take this instruction seriously because the risk of OHSS is high. OHSS causes the ovaries to become painful and swollen. In severe cases, this condition can be life-threatening.
Some couples are hesitant to “throw away” the cycle due to having too many follicles. However, if you have sex and conceive, you put yourself and your future babies at risk. Don’t do it.
Potential Challenges
IUI has helped many women become pregnant, but it doesn’t always work. In cycles where fertility drugs and IUI were combined, the pregnancy success rate can reach as high as 20%.5
These are per-cycle rates, meaning that the success odds are higher when looking at multiple cycles together. Often, it is recommended to commit to trying IUI for a minimum of three cycles.
Your personal success rate will vary depending on the cause of your infertility, the quality of the sperm you are using, and your age.
In a study of about 1,000 IUI cycles, researchers found that the success rate per couple (over one or more cycles) was in large part dependent on the woman’s age, medical history, and specific fertility issues
Success rates per couple (over more than one cycle) in this study were:
55.6% for cervical factor infertility
47.4% for anovulation (problems with ovulation)
41.7% for male factor infertility
37.6% for oligospermia (low sperm count)
35.1% for unexplained infertility
13.4% for asthenospermia (poor sperm motility)
10.7% for endometriosis
Among those with unexplained infertility, just 4% of women got pregnant per cycle without fertility drugs.

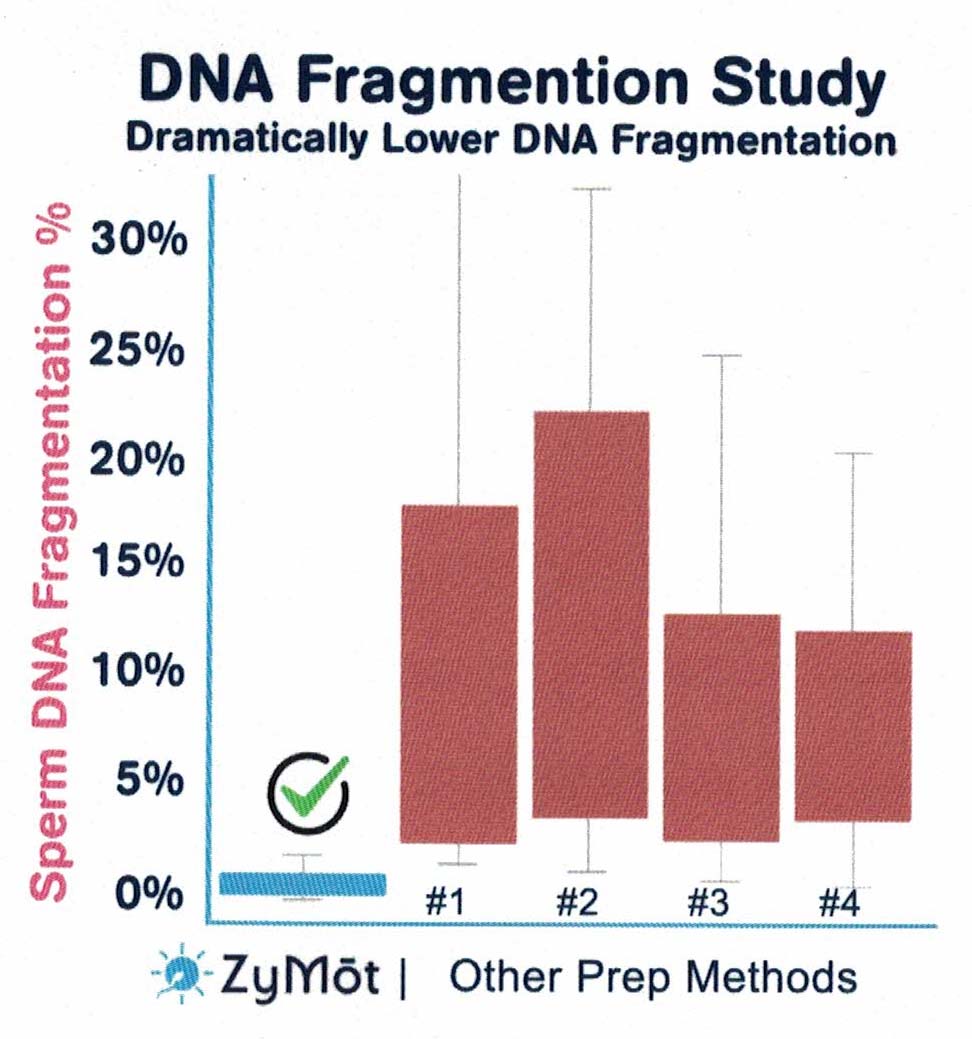
Did you know?
- Up to 50% of infertility cases are linked to poor sperm health
- Low sperm DNA fragmentation is a key factor of healthy sperm
- Selecting the healthiest sperm is possible with ZyM6t
ZyMot Sperm Separation Devices are an innovative, natural, simple way to isolate the healthiest, best-performing sperm with the lowest possible DNA fragmentation.
It’s science, baby!
Think you’re a good fit for Elements Brands? Jump right in with our team of creative, innovative and driven professionals that market, sell and manage our brands.
ZyMot separates and isolates the healthiest, best-performing sperm.
Sperm can have more than 35% DNA fragmentation, even for the healthiest of men.
DNA fragmentation indicates the presence of sperm with damaged (broken) DNA.
Integrity of sperm DNA is key to obtaining viable embryos, and subsequently a healthy baby. It’s just a fact of life.
Multiple independent studies have scientifically demonstrated that ZyMot Sperm Separation Devices isolate the best-performing sperm with the lowest-possible DNA fragmentation.
Intrauterine Insemination (IUI) Russian/Ukrainian Speaking Clinic for New Jersey patients
Study Findings
- In an independent study of 30 patients, ZyMot isolated the healthiest sperm with the lowest DNA fragmentation compared to commonly-used sperm preparation methods.*
- In another study at Weill-Cornell Medicine, ZyMBt delivered healthier sperm with the result being 21 live births/ongoing pregnancies versus zero births among the same couples who underwent standard sperm preparation.*
- In a study of 265 intrauterine insemination (IUI) patients with unexplained infertility, semen samples that were processed with ZyM6t resulted in patients being 3.5 times more likely to acheive an ongoing pregnancy than the age-matched control group with sperm that was processed via standard prep.*